Common factors within the gut associated with depression and bipolar disorder
New research has found that there is a common, overlapping environment in the gut bacteria of people living with mental illnesses like depression, bipolar disorder and anxiety.
The research, published in JAMA Psychiatry, found that people experiencing these illnesses are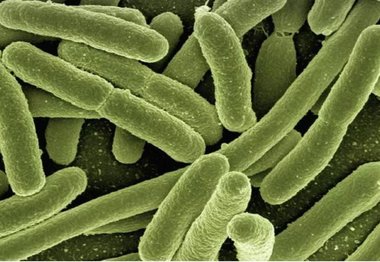 more likely to have gut biomes that are characterised both by a lack of anti-inflammatory producing bacteria, as well as a higher amount of proinflammatory bacteria.
more likely to have gut biomes that are characterised both by a lack of anti-inflammatory producing bacteria, as well as a higher amount of proinflammatory bacteria.
The research does not consider these biomarkers, but it does suggest that a greater awareness of gut health should be considered in the treatment of psychiatric disorders.
Gut microbiota is the large and dynamic community of microorganisms that live in the human gastrointestinal tract. This can include bacteria, viruses and fungi, as well as other types of microorganism. Previous studies have pointed to the important role that the gut microbiota plays in the development of mental illness.
In a diverse global sample, the investigators conducted a meta-analysis of 59 case-controlled studies looking at changes in the gut microbiome.
The study found that people experiencing depression, anxiety, bipolar disorder and psychosis were consistently found to have lower levels of faecalibacterium and coprococcus, two types of bacteria that have an anti-inflammatory effect within the gut. Further analysis found that individuals with these illnesses had higher levels of Eggerthella, a bacterium with pro-inflammatory effects.
Viktoriya Nikolova, the study’s first author from King’s College London Institute of Psychiatry, Psychology & Neuroscience, said:
The gut health of people living with depression, anxiety, bipolar disorder and psychosis all share common traits.
While we haven’t managed to establish biomarkers for specific illnesses, we have found that there is a significant overlap between gut health and the prevalence of mental illness, specifically in relation to the predominance of certain proinflammatory bacteria compared to anti-inflammatory bacteria.
Prof Allan Young, the study’s lead researcher from King’s College London Institute of Psychiatry, Psychology and Neuroscience, said:
To our knowledge, this is the first review to assess changes in the gut microbiota in relation to a range of psychiatric disorders and evaluate their potential as biomarkers. Our findings demonstrate that changes in the composition of the microbiota are widespread and, even though it is likely to be a lot more complicated than that, we see some indication of how they may be linked to other known underlying mechanisms of mental illness, such as the regulation of inflammatory processes. It is becoming more and more clear that the health of the gut microbiota is vitally important to the wider mental health of individuals.
This research was possible thanks to funding from the Medical Research Council (UK) and the National Institute for Health Research Maudsley Biomedical Research Centre.
Read the full paper: Perturbations in Gut Microbiota Composition in Psychiatric Disorders: A Review and Meta-analysis