6 December 2023
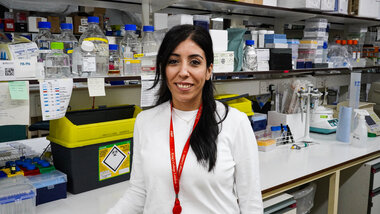
KHP went to visit Dr Sara El Hoss at the Red Cell Haematology Laboratory in the Rayne Institute, Denmark Hill. Dr El Hoss, a postdoctoral fellow at King’s College London, works on several research projects aiming to investigate the pathophysiology of sickle cell disease. She works very closely with medical doctors at King’s College Hospital NHS Foundation Trust.
Her research mission is tightly linked to education as she supervises students on various research projects. We learned about Dr El Hoss’s [pictured below] sickle cell disease research and her passion to find a cure for sickle cell disease, and how her upbringing in Africa shaped her research topic choices.
Why did you want to become a sickle cell disease researcher?
I knew sickle cell disease as a child because I was born and raised in Nigeria, the country that is home to the highest number of sickle patients. This was maybe the trigger.
I always knew I wanted to do research and work on sickle cell disease to find a solution, because I had friends and teachers at school who had sickle cell disease. When I started looking for a research field to specialise in, I knew I wanted to work on haematology because the blood always fascinated me. And I knew that I wanted to work on genetic disorders that are impacting the African population because I feel very connected to Africa as I lived there for 16 years. This is how I started working on sickle cell.
And the more I learned about the disease, the more I became passionate about it, and now I feel it's my mission to do something to help the African people, and in general to help sickle patients worldwide. We're in 2023 and we still don't have a cure suitable for all sickle patients yet. Nevertheless, it is important to mention that the UK approved the first gene editing treatment for sickle cell disease a few weeks after this interview was recorded, this is a huge break through and a step forward toward a better future for sickle cell patients globally.
This encouraging news is in line with my current projects as I am focusing on understanding how stem cells, the cells targeted by gene therapy, function in sickle cell disease. I do hope that my work will contribute just a little bit towards developing novel and improved treatments for sickle cell disease, and my dream is to be alive and witness a cure being proposed to every sickle patient in the world.
Please tell us about your research
 My research is focused on hemoglobinopathies, specifically sickle cell disease, one of the most common monogenic disorder in the world.
My research is focused on hemoglobinopathies, specifically sickle cell disease, one of the most common monogenic disorder in the world.
I’m trying to understand the pathophysiology of sickle cell disease – how the disease is happening and how complications are occuring in patients. The more we understand, the closer we will be to finding a cure, because we need to understand the mechanisms behind the disease to be able to develop treatments that could correct these mechanisms.
Sickle cell disease is a group of inherited red blood cell disorders, where patients will produce the sickle haemoglobin instead of adult haemoglobin causing the red blood cells to become sticky and stiff and look like a C shape, hence the name sickle.
As you can imagine, when red blood cell properties are impacted, the cells responsible for transporting oxygen in our body, all the organs get affected because our organs depend on the oxygen that's arriving via these red cells.
What we’ve learned during all these years working on sickle cell disease is that even though it is a genetic disease caused by a single point mutation, it is very complex, and it is capable of surprising us.
Until recently we always thought that the pathophysiology of sickle cell disease is happening in the circulation of the patient, but when we started investigating how sickle red cells are produced, we were able to discover new mechanisms that are impacted in sickle cell disease. My work focuses on studying the environment of the bone marrow niche, the place where red cells are produced.
 The process of red cell production is called erythropoiesis, during this process we have a stem cell that will commit and differentiate to become a young red blood cell, which then exits the bone marrow niche and goes to the circulation to mature and perform its job of delivering oxygen in our body.
The process of red cell production is called erythropoiesis, during this process we have a stem cell that will commit and differentiate to become a young red blood cell, which then exits the bone marrow niche and goes to the circulation to mature and perform its job of delivering oxygen in our body.
As I started investigating how erythropoiesis is occurring in sickle cell disease, I was able to pinpoint the stage at which the defect in this process starts in sickle cell. I therefore showed that this process is affected in sickle cell disease and that the bone marrow niche is also altered.
Why are our studies important? As new therapies including gene therapy aim to edit and correct the sickle mutation in the stem cells that are in the bone marrow niche, it is vital to investigate and characterise the niche in sickle cell disease. Moreover, what is still missing is that we don't know how these stem cells are impacted by the disease.
Therefore, my current and future research is now focusing on looking more at the niche, characterising the sickle stem cells, and investigating the process of erythropoiesis in sickle cell disease. This will allow us to understand how we can improve the delivery of gene therapy to the patients, and which patients will be more suitable for gene therapy.
This will hopefully direct the field towards a more precision medicine approach, that is having a tailored cure for each patient. I do believe that this is the way to move forward in curing sickle cell disease. Each patient should have a treatment tailored to them, and not all the patients should be treated in the same way.
On that subject, how do you see the future of sickle cell disease research?
 As I mentioned, I believe we're moving towards a direction of precision medicine - patients will be given treatment based on their disease history and what is more adaptable for them.
As I mentioned, I believe we're moving towards a direction of precision medicine - patients will be given treatment based on their disease history and what is more adaptable for them.
Hopefully in the future there will be more gene therapy research focused on prenatal or foetal gene therapies, which I think could be a very promising cure for sickle cell patients.
It is important to keep in mind that whatever treatment we develop for sickle cell must be cost effective. We cannot take treatments that are very expensive and imagine that they're going to be implicated in Africa. So, in parallel with focusing on cutting edge research, we also have to work with government entities, NGOs, charities and others to provide patients with the adequate healthcare in their countries.
We should move forward with anything that is curative, because to date we do not have a curative treatment for sickle cell except bone marrow transplantation, which has its limitation because you have to find a donor that matches with the patient. Unfortunately, this is not possible for all patients.
I think the future will be to find curative treatments and focus on a precision medicine approach, providing the patients with a personalised cure for them.
You can watch the video interview recorded with Dr El Hoss at her laboratory in the Rayne Institute below:
(1) KHP meets Dr Sara El Hoss, sickle cell disease researcher at King's College London - YouTube
To learn more about KHP Haematology, visit its webpages here.