10 May 2018
Dr Lucinda Gabriel, Darzi Fellow on the Value Based Healthcare programme, blogs about redesigning the orthopaedic clinical pathway to enhance value.
I joined King’s Health Partners as a Darzi Fellow in September 2017. I can’t believe I’m nearing the end of my 12-month project-based attachment so soon!
In my position with King’s Health Partners I have been working with orthopaedics leads across the partnership, including the Orthopaedics, Trauma and Plastics Clinical Academic Group to analyse end-to-end elective orthopaedics pathways as part of the Value Based Healthcare programme.
Watch Professor Moxham's video on how we're redesigning the orthopaedics pathway to improve value
https://
The challenge
My directive was to develop a ‘Value Calculator Toolkit’; an innovative methodology that would support our partners King's College London, and Guy's and St Thomas', King's College Hospital and South London and Maudsley NHS Foundation Trusts; as well as colleagues in primary and social care in Lambeth and Southwark and in Our Healthier South East London programme.
Now, if I’m honest, I wasn’t sure I knew what this was, let alone how I’d go about developing it. But I was assured that it could be done, and as Professor Moxham, Director of Clinical Strategy at King’s Health Partners, proclaimed, ‘it would be bloody brilliant!’
In our recent blog and videos Value Based Healthcare mini-series, value is defined as the relationship between outcomes and costs. To create a calculator I needed to better understand patient centred outcomes, relative to the true cost of delivering those outcomes.
The numerator
So, firstly, I began by looking at patient outcomes, the numerator in the equation. With the intention of keeping things relatively simple, a cohort of patients was identified with the help of Mr Toby Colegate-Stone, one of the orthopaedic surgeons at King’s College Hospital NHS Foundation Trust. 50 previously ‘fit and well’ patients who had undergone an elective hip replacement for primary osteoarthritis were selected. In orthopaedics, we are fortunate that a set of validated Patient Reported Outcome Measure Scores (PROMS) are already routinely collected at a national level. These provide an indication of a patient’s recovery after surgery in terms of their pain and function, and to a lesser extent their psychological well-being. For more about how we’re measuring outcomes in orthopaedics across our partnership, see the Orthopaedics, Trauma and Plastics Outcomes Book.
So, now we had outcomes, we needed to determine the denominator in the value equation. We needed to establish the costs.
The denominator
To do this, we had to work out what happened to patients. How did they enter the referral pathway? What investigations were undertaken? When were they admitted to hospital? What happened to them there and how long did they stay? And when they left? What sort of follow-up did they have? Was this in the community or did they return to the hospital? Who was involved in their care and what other costs were incurred?
With the help of the physiotherapists and medical staff, we mapped out the end-to-end pathway across the health system for the condition. We then approached the finance costing team, and the Business Intelligence Unit for input. Navigating the PLICS (Patient Level Information Costing System) can feel like learning a new language but with their help we were able to identify all the costs of care - including staffing and administrative costs, imaging, prostheses, medications, physiotherapy and occupational therapy costs.
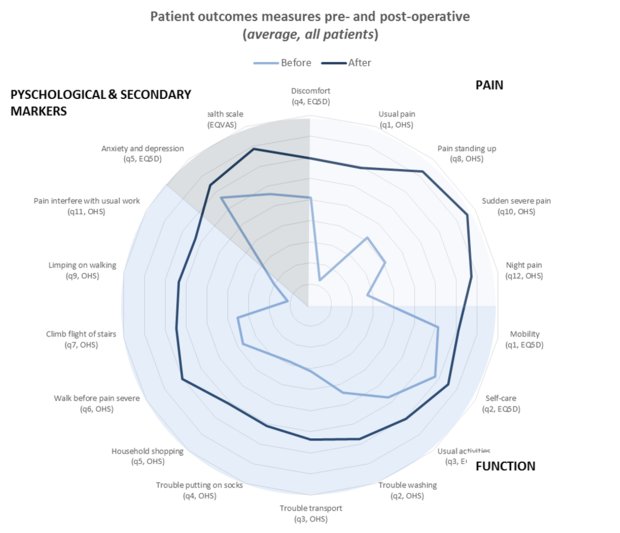
Image: The spider diagram shows the pre- and post- operative comparison of patient reported outcome measures (PROMs). The darker line shows the improvement in PROMs following surgery. The space between the lines represents the extent of improvement for each outcome measure. Oxford Hip Score (OHS), EQ5D and EQVAS (Visual Analogue Scale) are standardised instruments for measuring health status.
The calculator
Now we had some outcomes data, and some costing information. To make our results meaningful to clinicians and patients we used an outcomes framework. We rearranged the questions from each validated tool into domains of pain, physical function and psychosocial function. In this way, we could represent the post-operative scores graphically to demonstrate the level of improvement our cohort experienced.
Preliminary data is indicative only, but patients from King’s College Hospital were slightly older on admission and had more comorbidities than the Queen Mary Sidcup patients. Both groups showed a general improvement in patient reported outcome measure scores post-operatively. Although individual variation was more substantial, with some patients deriving great benefit from surgery and some being helped much less. Detailed costing information shows a large variation between patients and is still being refined following clinical review.
Next steps
The methodology of establishing accurate and relevant cost information across the partnership requires further work.
Currently the front-end of the pathway, prior to surgical referral, remains somewhat of a mystery. The key to moving forward will be to establish the additional costs incurred prior to being referred to a surgeon. This is a challenge but the rapid improvement in IT across our care system will soon make costing of the full pathway possible. We can then begin to work with clinical directors to quantify the potential impact that investment and disinvestment decisions could have on the end-to-end care pathway and inform the development of service changes both within King’s Health Partners and in Primary Care.
I am in the process of setting up some patient engagement activities to supplement the patient-centred metrics we currently have. Psychosocial outcomes especially are lacking and establishing outcomes that matter to patients and their carers will tie in with our work in the Mind & Body Programme. We will identify opportunities for embedding relevant mental health services within the orthopaedics pathway.
In the longer term, this work will facilitate the integration of care across local primary, secondary and social care services and make it easier for people to get the care and support they need with positive effects for the local health economy by achieving better outcomes with the money available (better value).
As the programme progresses and we realise some of these goals, we will work with health economists, implementation scientists and our Clinical Academic Groups to develop similar toolkits that will enable clinicians and managers to understand and apply value principles to other pathways in their quality improvement work.
To ensure that capacity in Value Based Healthcare is developed and owned by those responsible for implementing change, we will actively promote co-production by working closely with stakeholders within other specialties to ensure that outputs from the toolkit are understood and meaningful to all healthcare professionals. Along the way we hope to develop leadership and organisational skills among trainee doctors and other healthcare professionals within King’s Health Partners.
Reflections
I have really enjoyed the multidimensional aspect to this work. I have the freedom to engage with multidisciplinary clinical teams, trust transformation programmes and commissioning bodies to identify how the value methodology can be applied to improve patient outcomes, while considering sustainability within the local health economy. It is an exciting time in the NHS with so many new initiatives; the existing Change Programmes within trusts, NHS values, the Five Year Forward View and the Sustainability and Transformation Partnerships. This role has given me the opportunity to gain a working knowledge of the health and care system whilst simultaneously, by way of the Darzi Fellowship, gaining an understanding of the theoretical underpinnings of change implementation, process improvement and management across organisational boundaries and the wider health and care economy.
It will be exciting to see how the Value Based Healthcare and Mind & Body programmes evolve, and how they can be integrated further as we move forward.
Read more about Value Based Healthcare.
Check out our Value Based Healthcare mini-series.





