18 September 2018
Professor John Moxham, Director of Clinical Strategy, King’s Health Partners, blogs about measuring, recording and controlling five key measures - the Vital 5 - to improve value and reduce health inequalities.
At the heart of understanding how we can increase value (achieve best possible outcomes for all patients with the resources available) is understanding and then improving the complete pathway of diseases and their treatment. However, the fragmentation of our healthcare system has meant that such an approach has seldom been attempted or achieved.
Watch Professor Moxham's introduction to the Vital 5
For many diseases, including most of the long-term conditions threatening to overwhelm the NHS, the initiation and development of those diseases is a consequence of a relatively small number of behaviours and conditions. Of particular importance are high blood pressure, obesity, smoking, alcohol and common mental health conditions. Those patients with poor mental health often also have physical health problems and many patients with chronically poor physical health frequently also have mental health conditions. Few diseases can be properly managed without consideration of both mind and body.
King's Health Partners believes that reducing obesity, smoking, harmful drinking, controlling blood pressure, and identifying and improving poor mental health - what we have termed the Vital 5 - would strengthen multiple care pathways and massively increase value.
Identifying, recording, and sharing Vital 5 data between all health partners and our patients and acting on the results across our population, would substantially improve outcomes and make our health and care system more sustainable. Our ambition is to have a digital scorecard of the Vital 5 within routine clinical notes. The scorecard will be shared both with the patients and all the clinicians caring for them, prompting supportive interventions.
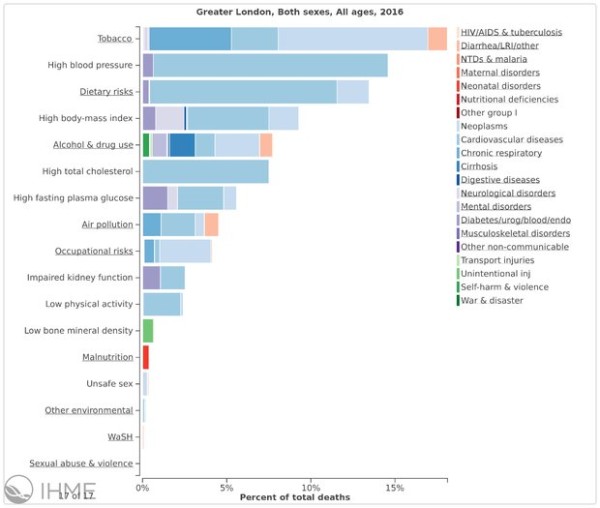
The Vital 5 all have a major impact on the burden of disease (UK results), whilst the graph below reflects the percentage of deaths by cause and condition for the Greater London area (Greater London results, risks by cause), both as presented by the Institute for Health Metrics and Evaluation.
High Blood Pressure causes vascular disease and therefore strokes, heart attacks, heart failure, kidney failure and contributes to dementia. It is commonly underdiagnosed and poorly controlled. Good guidelines for treatment are available, but adherence is a challenge, particularly for patients with mental health conditions. Exercise and losing excess weight are important aspects of successful treatment (British Heart Foundation).
Obesity is the main cause of type 2 diabetes and its complications, including the need for dialysis, leg and foot ulcers, and amputations. It is an increasingly important cause of liver disease, failure and need for transplantation. Obesity is the second leading cause of cancers (6%), after smoking (15%), and causes at least 13 types of cancer: oesophageal, stomach, bowel, liver, pancreas, gallbladder, breast, uterus, ovary, kidney, thyroid, myeloma, and meningioma (Cancer Research UK).
Excess Alcohol consumption causes accidents, violence, mental health conditions, brain damage, liver disease and need for transplantation, heart disease, gastrointestinal disease, oesophageal, and gastric cancer. Alcohol misuse is the biggest risk factor for death, ill-health and disability among 15-49 year-olds in the UK, and the fifth biggest risk factor across all ages (Alcohol Concern UK).
Smoking is the single biggest avoidable risk factor for cancer. It is a major cause of heart and circulatory disease (25,000 deaths in the UK each year) and chronic disabling lung disease. There is a growing body of evidence to suggest that smoking is an independent risk factor for diabetes and that it raises the chance of developing dementia by 50%, versus those who have never smoked (Action on Smoking and Health).
Mental health conditions are often accompanied by poor physical health, which greatly reduces life expectancy. Mental health conditions, usually anxiety and/or depression, are present in 30% of patients with physical ill health, making treatment of physical illnesses more difficult. Good treatment of any long-term condition requires assessment of mental health, which can be done using available mental health assessment scores (King’s Health Partners Mind & Body).
Delivering progress on the Vital 5 will require a substantial cross-system collaborative effort.
King’s Health Partners is therefore working closely with our partners, as well as with general practice and primary care organisations, Public Health England, and the South East London Sustainability and Transformation Partnership (Our Healthier South East London). We are also working closely with our health and care commissioners. As a start, commissioners have developed a Health Improvement Commissioning for Quality and Innovation contract (CQUIN) with King’s College Hospital and Guy’s and St Thomas’ NHS Foundation Trusts to make progress on the recording and sharing of information on the Vital 5. This will build on national alcohol and smoking CQUINS as well as Making Every Contact Count and our Integrated Mental & Physical healthcare: Research, Training & Services project, as part of our Mind & Body programme.
Given the imperative of needing to substantially increase value across the health and care system we believe the Vital 5 programme will make a significant contribution.
Read more about Value Based Healthcare at King's Health Partners.